Celiac disease is a chronic autoimmune disorder triggered by the consumption of gluten, a protein present in wheat, barley, rye, and, in some cases, oats that have been contaminated. Although it primarily damages the small intestine, the condition can also cause symptoms in other parts of the body. This disease develops in genetically predisposed individuals when their immune system reacts abnormally to gluten, leading to inflammation and long-term complications if left untreated.
When someone with celiac disease consumes gluten, the immune system triggers an abnormal response that inflames and damages the intestinal villi, the tiny structures responsible for nutrient absorption. As a result, the body can experience malabsorption, nutritional deficiencies, and even systemic complications if the condition is not properly managed.
The disease is estimated to affect approximately 1% of the world’s population although many cases remain undiagnosed due to the variety and sometimes absence of its symptoms.
Causes and risk factors
The exact cause of celiac disease is still unknown, but research suggests it results from a combination of genetic, environmental, and immune system factors. Although the condition is not directly inherited, having a genetic predisposition is essential for its development.
Genetic factors
Most people with celiac disease carry the HLA-DQ2 and/or HLA-DQ8 genetic variants on chromosome 6, which are linked to immune system function. Over 95% of patients have HLA-DQ2, and nearly all others carry HLA-DQ8. However, having these genes alone does not guarantee developing the disease, since 30–40% of the general population also carry them without becoming celiac.
Environmental factors
In addition to genetic predisposition, it is believed that the following factors are necessary environmental triggers that activate the abnormal immune response to gluten. However, these environmental factors have not yet been conclusively demonstrated. Among the most studied are:
✅ Early gastrointestinal infections: some research suggests that certain viral infections, such as rotavirus or enterovirus in infancy, may alter intestinal permeability and promote abnormal immune response to gluten in predisposed individuals.
✅ Timing of introduction of gluten into the infant diet: It was formerly believed that the introduction of gluten at a specific time during complementary feeding could influence the risk of celiac disease. Recent studies have questioned this hypothesis, but it is still under investigation whether the amount and the context (presence of breastfeeding, simultaneous infections) play a modulating role.
✅ Other immunological and environmental factors still under study: aspects such as the gut microbiome (beneficial bacteria and their balance), early antibiotic use, type of delivery (cesarean vs. vaginal), exposure to environmental pollutants or immune stress at critical stages of development are being explored.
Increased risk in family members and other autoimmune diseases
Celiac disease is more common among first-degree relatives of patients, with a risk of about 10% compared to 1% in the general population. For this reason, guidelines recommend screening siblings, children, and parents, even if they show no symptoms.
In addition, celiac disease is more common in people with other autoimmune diseases, such as:
- Diabetes mellitus type 1.
- Autoimmune Thyroiditis (Hashimoto’s or Graves’).
- Addison’s disease.
- Sjögren’ syndrome.
- Dermatitis herpetiformis.
This association suggests a common immunogenetic background and makes it necessary to maintain a high index of clinical suspicion in these at-risk groups.
Conclusion on causes and risk factors
Therefore, although genetic factors are necessary, celiac disease is not inherited simply, but as a combination of predisposition and environmental exposure. The identification of these elements could, in the future, open the door to risk prevention or modulation strategies.
Symptoms of celiac disease
One of the biggest challenges in celiac disease is its clinical heterogeneity. There are people with typical digestive symptoms, others with extraintestinal manifestations, and even some asymptomatic.
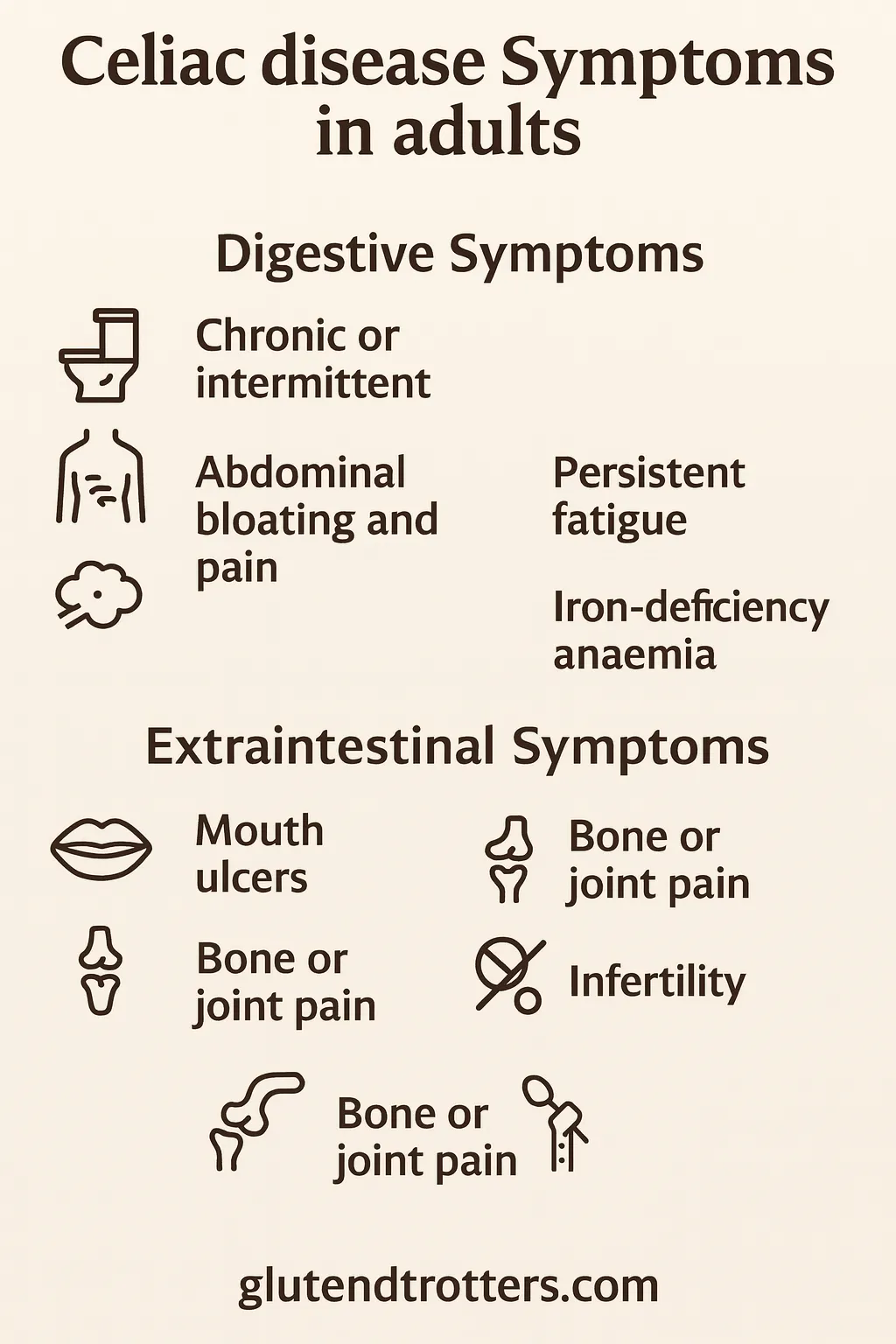
Symptoms in adults
In adults, celiac disease can remain undiagnosed for years, since symptoms are often subtle or atypical compared to the classic childhood presentation. As a result, many adults receive their diagnosis only after consulting multiple specialists or undergoing tests for unrelated conditions.
Digestive symptoms of celiac disease are often confused with conditions like irritable bowel syndrome, lactose intolerance, or other functional disorders. That’s why it is essential to recognize its most frequent manifestations:
Digestive symptoms
- Chronic or intermittent diarrhea: one of the most common symptoms, although not always present. In some cases, diarrhea alternates with episodes of constipation, making diagnostic suspicion difficult.
- Bloating and abdominal pain: many people report a feeling of bloating after meals, accompanied by abdominal discomfort or cramping.
- Excessive flatulence: increased gas is frequent due to fermentation of unabsorbed carbohydrates in the affected intestine.
- Occasional nausea and vomiting: less common, but possible in early stages or after accidental exposures to gluten.
- Weight loss without apparent cause: occurs due to malabsorption of nutrients. Some people also have decreased appetite.
Extradigestive symptoms
In adults, manifestations outside the digestive tract are very frequent and often the only ones present, contributing to the delay in diagnosis:
- Persistent fatigue: feeling of generalized tiredness that does not improve with rest, linked to nutritional deficiencies.
- Iron deficiency anemia resistant to oral iron: one of the most frequent signs, which does not respond to treatment until gluten is excluded.
- Osteopenia or early osteoporosis: Due to malabsorption of calcium and vitamin D, increasing the risk of fractures.
- Recurrent mouth ulcers or aphthous ulcers: painful lesions on the oral mucosa, not attributable to other causes.
- Bone or joint pain: diffuse discomfort without demonstrable inflammatory cause.
- Infertility or recurrent miscarriages: in women, untreated celiac disease can affect fertility and increase the risk of obstetric complications.
- Neurological alterations: such as peripheral neuropathy (tingling, loss of sensitivity in hands and feet) or ataxia (balance and coordination problems).
In addition to these symptoms, some adults show asymptomatic forms of celiac disease, detected only through findings such as:
- Blood tests requested for persistent anemia.
- Tests performed in first-degree relatives of celiac patients.
- Study prior to bone marrow donation or in systematic screening.
👉 It is important to note that atypical forms are not without risk: even if there are no obvious symptoms, intestinal damage and long-term complications can still develop if a gluten-free diet is not followed.
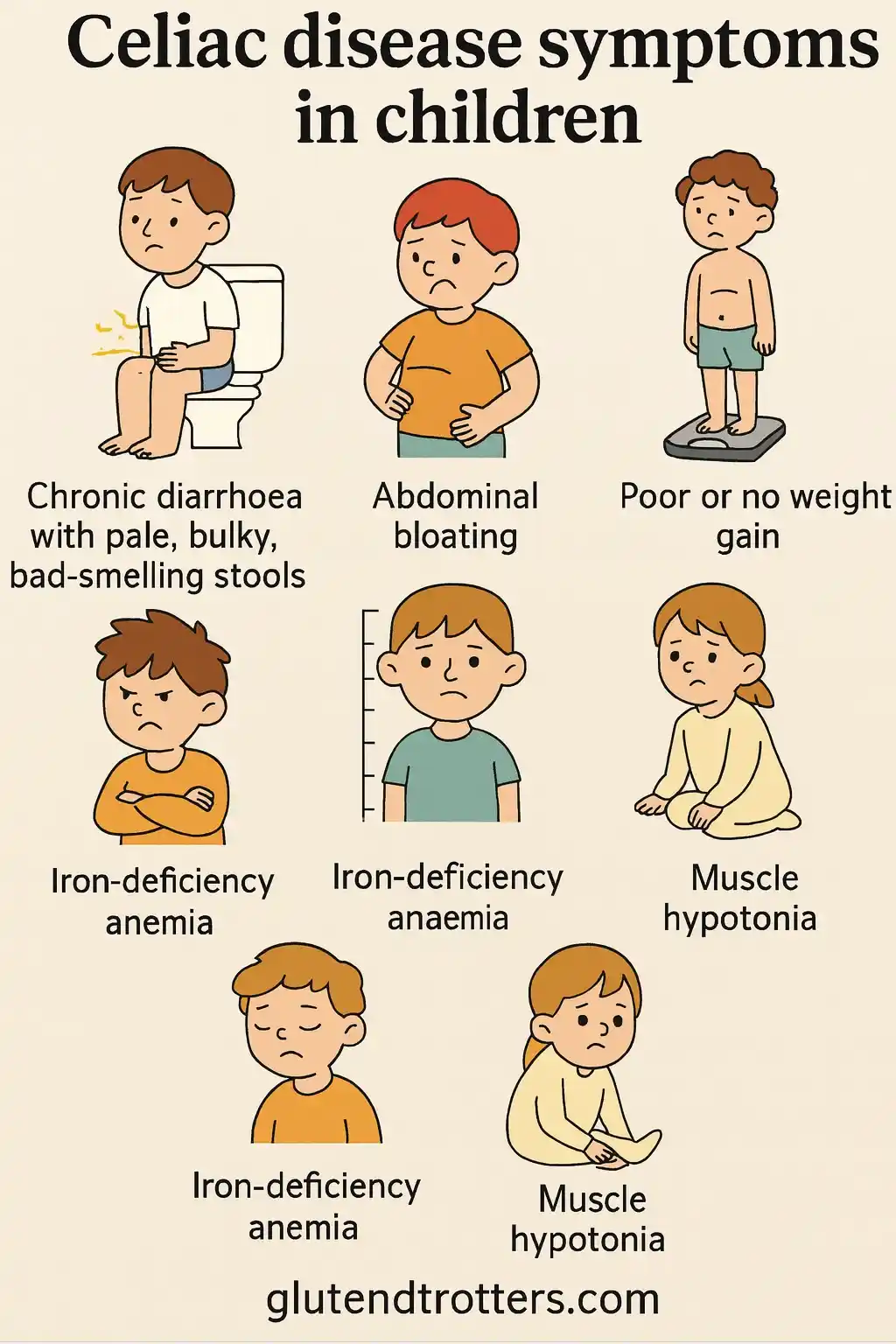
Symptoms in children
In childhood, celiac disease typically develops after gluten is introduced into the diet. The first symptoms often appear weeks or months later and are linked to the intestine’s impaired capacity to absorb nutrients. This malabsorption can lead to issues such as poor growth, abdominal bloating, diarrhea, or irritability, which are considered the classic signs of the disease in children.
In fact, this was the case with my daughter Manuela, who was diagnosed with celiac disease at the age of one. After introducing gluten into her diet, she began to experience abdominal bloating with pain, loose stools, and noticeable weight loss. These symptoms led us to consult the pediatrician and, after the necessary tests, the diagnosis was confirmed. From that moment, we adopted a strict gluten-free diet, which allowed her to quickly regain both weight and vitality.
Most common digestive symptoms in young children
✅ Chronic diarrhea with bulky, foul-smelling, greasy stools: known as steatorrhea, is a consequence of poor absorption of fats. Stools are usually pale, with a very unpleasant odor and difficult to clean.
✅ Abdominal distention (protruding abdomen): the child’s belly looks swollen and protruding, despite having slender limbs, due to increased intestinal gas and weakness of the abdominal musculature.
✅ Loss or poor weight gain: despite apparently adequate caloric intake, the child loses weight or does not progress on the growth curve.
Other common symptoms in childhood
✅ Irritability, apathy or mood swings: children may appear irritable, apathetic or low interest in play, reflecting general malaise or fatigue.
✅ Stunting and short stature: failure to thrive is one of the most important signs; children do not reach the expected heights for their age and lose growth percentiles.
✅ Iron deficiency anemia: intestinal malabsorption causes iron deficiency, manifested as pallor, fatigue or reduced physical and school performance.
✅ Muscle hypotonia: some children have low muscle tone, which affects their posture, balance and motor development.
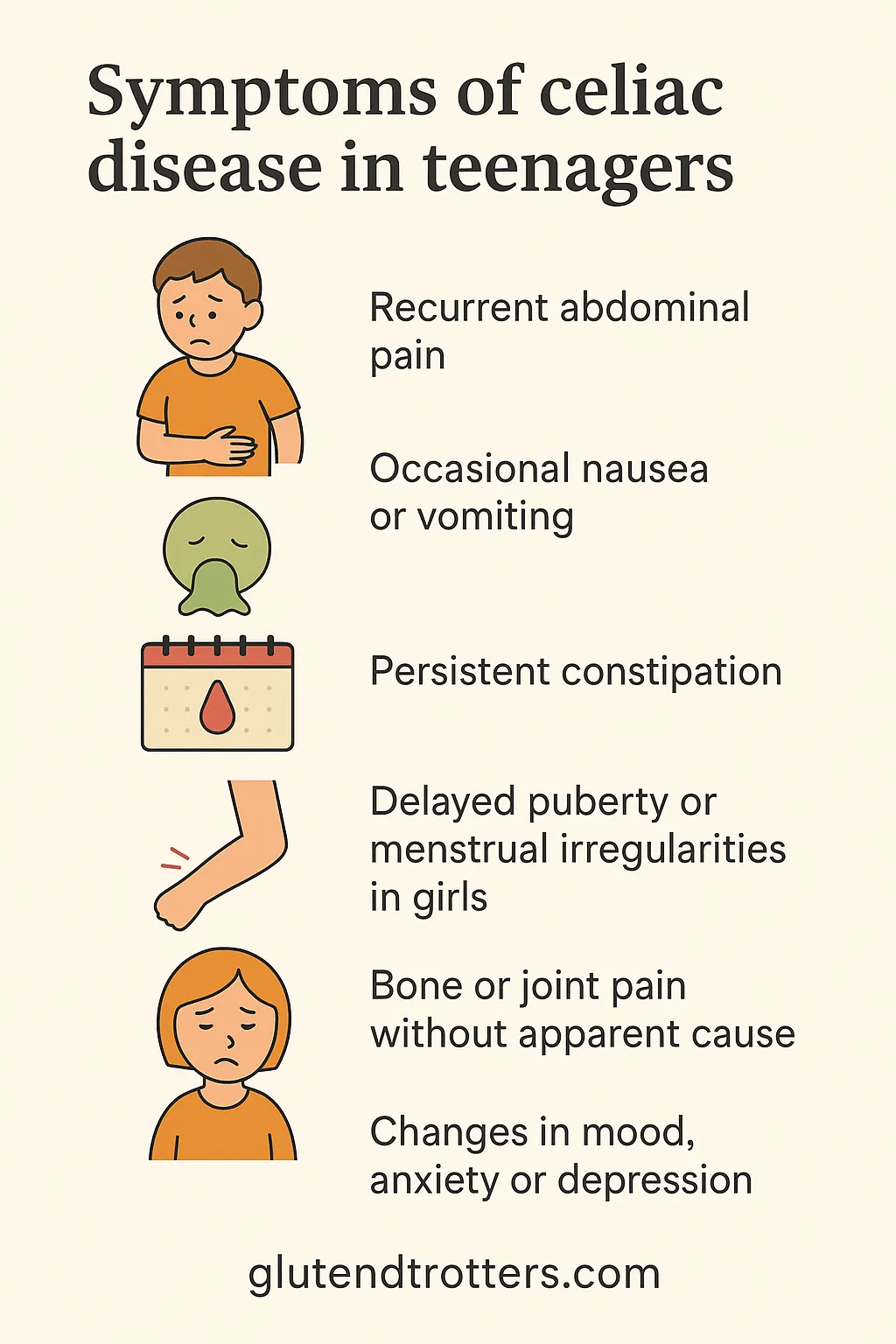
Symptoms in older children and adolescents
In older children and adolescents, symptoms may differ from the classic picture and be more subtle, making early diagnosis difficult. In these cases they may appear:
- Recurrent abdominal pain, colic type.
- Occasional nausea or vomiting.
- Persistent constipation, rather than diarrhea.
- Delayed puberty or menstrual irregularities in girls.
- Bone or joint pain without apparent cause.
- Changes in mood, anxiety or depression.
Atypical forms of the disease
As in adults, some children present with atypical forms of the disease without obvious digestive symptoms.
👉 It is essential to be alert to for extra-digestive symptoms in infancy, as up to 50% of children may not have diarrhea or typical digestive symptoms.
Importance of early diagnosis
Early diagnosis in infancy is key to avoid nutritional complications, bone development problems and other long term nutritional complications, bone development problems and other long-term alterations.. The exclusion of gluten from the diet after diagnosis usually results in a rapid improvement of symptoms and a recovery of growth in most cases.
Diagnosis of celiac disease
The diagnosis of celiac disease involves a combination of serological, genetic, and histopathological tests, which must be carried out while the person is still consuming gluten (except in rare cases).
Serological tests
The first diagnostic step is antibody testing:
- Anti-tissue transglutaminase antibodies (tTG-IgA): more sensitive and specific initial test.
- Anti-endomysial antibodies (EMA): useful as a confirmatory test.
- Determination of total IgA: to rule out IgA deficiency that falsifies results.
- Anti-gliadin deaminase antibodies (DGP): used in certain pediatric contexts.
A positive result indicates high probability, but is not a substitute for biopsy.
2. Genetic studies
The genetic test identifies the presence of HLA-DQ2 and HLA-DQ8. Its absence practically rules out the disease; its presence increases the probability, but does not confirm.
It is useful in doubtful cases or in first-degree relatives.
3. Intestinal biopsy
Definitive diagnosis usually requires a duodenal biopsy by endoscopy, which shows:
- Atrophy of the intestinal villi.
- Crypt hyperplasia.
- Increase of intraepithelial lymphocytes.
In some children with clear symptoms and very high antibody titers, current guidelines allow dispensing with biopsy under strict criteria.
Treatment of celiac disease
Currently, there is no cure. The only effective treatment is a strict and lifelong gluten-free diet. Eliminating gluten allows the regeneration of intestinal villi and the disappearance of symptoms.
Foods to avoid:
❌ Wheat, barley, rye and derivatives.
❌ Breads, pastas, flours, pastries, commercial cereals containing gluten.
❌ Processed products not certified gluten-free (due to risk of cross-contamination).
Safe gluten-free food:
✅ Fruits, vegetables, legumes, natural nuts.
✅ Fresh, unprocessed meat and fish.
✅ Eggs, dairy products with no additives.
✅ Rice, corn, quinoa, buckwheat, amaranth.
Also read: List of Gluten-Free Foods
The label reading is essential to avoid hidden gluten. In addition, it is key to prevent cross-contamination in kitchens and restaurants.
Also read: Celiac Cross-Contamination: What It Is, Main Risks and How to Prevent It
Adherence and follow-up
Follow-up includes:
- Periodic analytical controls.
- Antibody monitoring.
- Evaluation of intestinal mucosa recovery.
- Continuing dietetic education.
Adherence to the diet improves quality of life and prevents complications such as intestinal lymphomas, osteoporosis, infertility or neurological disorders.
Also read: Starting a Gluten-Free Diet: Key Benefits and How to Avoid Beginner Mistakes
Living with celiac disease: challenges and support
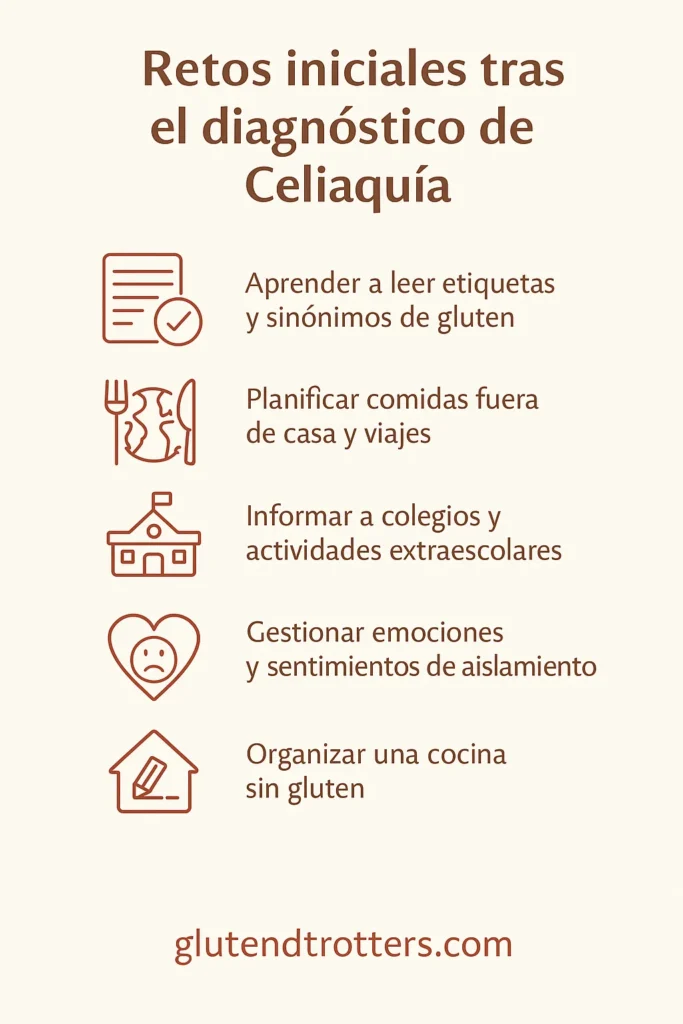
The diagnosis of celiac disease brings important changes to daily life, especially during the first months after receiving it. Adapting to a gluten-free diet means not only modifying what you eat, but also adjusting your mindset and daily organization. For many families this transition can feel overwhelming at first, but with time it becomes part of a new normal.
Initial challenges after diagnosis
Some of the most important challenges at the beginning include:
✅ Learn to read labels and know synonyms for gluten in ingredients: a critical step in identifying potential sources of hidden gluten in processed products and avoiding unintentional errors. Over time, this skill becomes automatic, but it can be complex at first due to the number of technical terms and alternative names for gluten.
✅ Organize a safe gluten-free kitchen: one of the first steps after diagnosis is to adapt the kitchen to avoid cross-contamination. This involves separating utensils, labeling products, cleaning surfaces appropriately and, in many cases, doing a little “logistical rearranging” in cupboards and pantries.
Also read: how to organize a gluten-free kitchen.
✅ Planning meals away from home and travel: Eating out or traveling with celiac disease requires extra planning and preparation. This very need to organize ahead was one of the main reasons we created Glutendtrotters: to support others with celiac disease in finding safe options at different destinations and to prove that gluten-free travel is not only possible, but also enriching. Also read: 7 Gluten-Free Travel Tips and Guide for Celiacs.
✅ Inform and train schools, canteens and extracurricular activities: in the case of celiac children, it is imperative to communicate dietary needs to the school and social environment, ensuring that they can safely participate in all activities.
✅ Managing emotions and possible feelings of frustration or social isolation: it is normal for fears to arise at first about how the disease will affect social relationships, celebrations or activities with other children.
Our personal experience
However, in our personal experience, we have always felt very supported. Except for a few isolated situations, Manuela has never faced social exclusion; on the contrary, both at school and during our trips, we have consistently met people willing to help.
I especially remember a moment in Marrakech, when Mohammed, one of the receptionists at the riad where we were staying, would go out every morning to buy gluten-free yogurts for Manuela. Since the traditional breakfast at the riad wasn’t safe for her or for my husband, this simple gesture became a true example of empathy and hospitality, reminding us that even far from home, we were not alone.
The role of social support and partnerships
Social support is essential for maintaining adherence to the gluten-free diet and fostering emotional well-being, especially in children. Celiac associations play a vital role by offering updated information, personalized guidance, cooking workshops, directories of safe restaurants, and digital tools such as apps and product guides.
In our case, the first thing we did after receiving the diagnosis was to get in contact with the Celiac Association of Cantabria (ACECAN). They gave us all the information we needed, guided us through the first steps, and answered our questions during those first days when we felt completely lost. That’s why we always recommend newly diagnosed families to contact the celiac association in their region; their support and experience are invaluable during this stage of adaptation.
A full and safe gluten-free life
Over time, we have learned that although living with celiac disease requires effort and attention, it does not stop us from leading a full, active, and happy life. With the right information, support, and planning, it is entirely possible to enjoy food, travel, and social experiences without compromising safety.
Conclusion
Celiac disease is a complex autoimmune disease, which requires a strict gluten-free diet to control symptoms and avoid complications.
Early diagnosis, proper follow-up and psychosocial support are essential to ensure a good quality of life. Thanks to growing social awareness and improved product offerings, it is becoming easier to live gluten-free. On the other hand, it is also true that challenges persist in social and travel environments.
Rigorous information, dietary education and professional and community support are key allies on this path.
Related Posts:
- Best Diet for Hypothyroidism: Complete Guide, Real Experience, and Practical Tips
- Best Gluten-Free Flours for Every Recipe: Complete Guide to Benefits and Uses
FAQs
Celiac disease involves a genetic predisposition that, when exposed to gluten, generates an abnormal immune response with intestinal damage.
No. The only way to control the disease is to completely eliminate gluten from the diet.
It has an important hereditary component. First-degree relatives have a 5-10% risk.
Yes. Although it is most common in childhood, it can develop at any age.
Oats uncontaminated may be tolerated in some people under medical supervision.
Sources consulted
- MedlinePlus. Celiac disease.
- University of Navarra Clinic. Celiac disease.
- Mayo Clinic. Celiac disease: symptoms and causes.
- NIDDK. Treatment of celiac disease.
All contents related to diseases or other pathologies present in our articles have exclusively an informative and divulgative purpose. It is essential to understand that the information provided in these materials is not intended, at any time, to replace the professional diagnosis of a physician or other health specialist. In case of any concerns or doubts about your health condition, we strongly urge you to contact your primary care physician or a medical specialist immediately. These professionals have the training and experience to make accurate assessments and provide case-specific medical guidance. It is important to note that no member of Glutendtrotters assumes any responsibility for decisions made or clinical situations arising from reading our articles. The information provided here should not be considered a substitute for personalized, professional medical advice.
